Journal of the NACAA
ISSN 2158-9429
Volume 7, Issue 2 - December, 2014
Recommendations for Extension Professionals and Volunteers Regarding Individuals with Delusional Infestation
- Kerr, S. R., WSU NW Regional Livestock And Dairy Extension Specialist, Washington State University
Glass, J. R., Plant Diagnostician, WSU Puyallup Plant & Insect Diagnostic Laboratory
Collman, S. J., Horticulture and IPM Educator, WSU Snohomish County Extension
Bush, M. R., Extension Entomologist, WSU Extension-Yakima County
Pehling, D. J., Extension Educator, WSU Extension-Snohomish County
Murray, T. A., County Director, WSU Extension-Skamania County
ABSTRACT
Delusional Infestation is a psychological condition wherein someone feels and believes insects or parasites are present on their body and/or infest their home. This “sensation” may lead sufferers to cause visible self-trauma to their skin. Such persons often seek assistance from Extension professionals or volunteers who provide diagnostic services. These clients may become agitated when Extension services are unable to identify the cause or doubt there is an infestation. Extension personnel likely to encounter such sufferers should become knowledgeable about Delusional Infestation. Extension offices should have a protocol for training volunteers and dealing with such cases.
Introduction
Delusional Infestation (DI, also called Delusory Parasitosis, Parasitophobia, and Ekbom Syndrome) is a psychological condition wherein those afflicted believe and sense insects, parasites, mites or “bugs” are present in or on their bodies and/or infest their environment (Trabert, 1995). Initial complaints from these sufferers include itchy skin, the sensation of being bitten by something, tingling skin, and other abnormal skin sensations (Hinkle, 2011). As the condition progresses, sufferers may develop skin lesions as a result of scratching and other self-induced trauma.
This condition is not a phobia because sufferers do not necessarily have an abnormal fear of insects. Although DI is considered rare in the general population, Washington State University Extension receives one or two people statewide each month who express conditions consistent with delusional infestation (Todd Murray, personal communication, August 21, 2014). Afflicted persons repeatedly seek help from various sources including health professionals, entomologists, pest control professionals, veterinarians, and Extension personnel (Hinkle, 2000). In a study of 23 cases, Boggild et al. (2010) reported each patient visits an average of 6.3 + 3.5 health care providers when seeking relief from DI. Although diagnostic investigations fail to isolate any causative organisms, the complainant’s claims persist. This is the definition of a delusion--a persistently false belief maintained despite evidence to the contrary. Inability of a specialist to find a cause is often interpreted by the patient as incompetence (Freudenmann & Lepping, 2009; Munroe, 1988). Then again, a negative finding is not definitive proof that pests do not exist.
This issue is a potential concern for Extension personnel because it is a long-term condition with a poor likelihood of resolution without appropriate therapy (Koblenzer, 2010); also, those afflicted can become agitated if challenged (Freudenmann & Lepping, 2009). Extension personnel and volunteers often have no awareness of the affliction and usually have no training about how to recognize or deal with this condition. To exacerbate the level of the frustration, there are multiple causes of skin irritations and many are difficult to diagnose by visual examination alone.
Typical Presentation
Cases of DI increase with age and are about twice as common in older women than men (Trabert, 1995; Boggild et al., 2010; Lyell, 1983; Wykoff, 1987). However, DI may be associated with abuse of alcohol, amphetamines, methamphetamine, and cocaine (Munro, 1988; Yeh et al., 2014; Frieden, 2006; Trabert, 1995); younger people are more often in this category. Some cases are associated with recent or chronic stressful situations such as divorce, displacement from a home, unemployment, death of a loved one, etc. (Fellner & Majeed, 2009; Lyell, 1983). No particular socioeconomic class is at increased risk for this condition (Boggild et al., 2010; Lyell, 1983).
As described by Freudenmann & Lepping (2009), primary DI has no underlying cause. Secondary DI can be found in conjunction with psychiatric conditions such as schizophrenia (Lee, 2008; Lyell, 1983) and organic brain disease such as dementia (Freudenmann & Lepping, 2009). Secondary DI can also be the result of substance abuse and numerous primary health conditions discussed below.
Whether primary or secondary, there are many signs and symptoms DI sufferers often have in common. Suspected DI sufferers may willingly show parts of the body not normally exposed to strangers. Self-mutilation is very common, either secondary to intense scratching or physical trauma to the skin to “let the bugs out” (Lyell, 1983). Lesions include excoriations, scratches, scabs, ulcers, pigmentary changes, bruising, redness, and thickened skin (Lee, 2008; Fellner & Majeed, 2009; Freudenmann & Lepping, 2009; Boggild et al., 2010; Hinkle, 2011). Sufferers may list the many substances with which they have treated themselves and their environment. Their skin may also be secondarily affected by frequent bathing and scrubbing and the use of harsh chemicals such as pesticides, vinegar, bleach, gasoline, and alcohol (Lyell, 1983; Hinkle, 2000). Real dermatitis, whether self-induced or a result of chemical treatment, makes the condition a self-fulfilling prophecy: scratching begets irritation which begets itching and a strengthened belief the skin is infested with bugs (Freudenmann & Lepping, 2009). Those afflicted with DI may even recruit other family members into their delusion; indeed, having multiple family members affected at the same time is not unusual (Lyell, 1983; Lee, 2008).
A typical DI sufferer will bring many containers of “samples” on their first or subsequent visits seeking help (Figure 1). These samples may contain skin scrapings, floor sweepings (Figure 2), lint, paper, clothing, bedding, or used bath water (Fellner & Majeed, 2009; Lee, 2008; Lyell, 1983). This action is such a common characteristic of the condition that Freudenmann & Lepping (2009) call it “the specimen sign."

Figure 1. The specimen sign: example of “sample” over-submission by presumed DI client. Photo courtesy of Jenny Glass.

Figure 2. Typical example of sample submitted by presumed DI client. Contents include pet hair, human hair, dirt, plant material, paper scraps, beads, popcorn kernel, sunflower seed, pet toenails and feathers. Photo courtesy of Susan Kerr.
Clients will repeatedly seek advice from a range of health and service providers (Munro, 1988), sequentially rejecting the non-findings of each consultant as they search for someone to identify and diagnose the “bug” responsible for their symptoms. In some cases, complainants will claim the insects are invisible (Hinkle, 2011; Lyell, 1983). In other cases, the claim is made that the parasite will change color or behavior. Indeed, many sufferers can describe complex life cycles of their invisible pests in great detail (Lee, 2008; Lyell, 1983). These life cycles sometimes defy logic, giving pests the characteristic of facultative parasitosis--the ability to live off both inorganic material and humans (Hinkle, 2011). Some of those afflicted have a hallucinatory component to their syndrome (Munro, 1988) and insist they can see the causative agents coming out of their skin (Mehmood & Khasawneh, 2014) or from solid objects such as fireplaces and stoves.
The lives of those suffering from DI can become quite desperate. Social isolation is an initial risk factor in these cases (Trabert, 1995; Lyell, 1983) and those so afflicted often create increasingly-isolated lives to protect their loved ones from exposure (Boggild et al., 2010; Lyell, 1983). Many engage in frequent and fervent cleaning efforts of themselves and their home (Freudenmann & Lepping, 2009). They can destroy possessions, clothing, bedding, furniture, etc. in a misguided effort to eliminate the source of the problem (Hinkle, 2011; Lyell, 1983). Interestingly, in primary DI, this is their only delusion. These clients do not display other odd behaviors or additional abnormalities (Freudenmann & Lepping, 2009; Wykoff, 1987).
Although the clinical form of DI is rare in the general population, there is a plethora of conditions and organisms that can cause the sensation of bites or development of skin irritations. The sensation can be initiated by an actual agent (Lee, 2008; Lyell, 1983)—such as biting fleas or northern fowl mites—and become self-perpetuating as the sufferer scratches the skin. Other actual pests can go unnoticed for quite some time. In urban areas, tropical rat mites may feed on human hosts while residing in unnoticed rat habitat. Northern fowl mites can migrate from abandoned bird nests and feed on nearby human hosts. In some cases, the sensation of skin irritation can persist after resolution of the inciting cause (Lee, 2008).
Identifying the cause of “itchy skin” can be maddeningly difficult. Dermatologists and/or internists may begin their diagnostic workups with physical examination and tests to rule out known causes of human skin irritation including contact dermatitis, dry environments, liver disease, diabetes, vitamin deficiency, medication reactions, allergies, hypothyroid disease, ringworm, cancer, and other diseases (Lee, 2008; Freudenmann & Lepping, 2009; Koblenzer, 2010). There are biting pests Extension personnel and volunteers (such as Master Gardeners) can rule out including fleas, ticks, lice, chiggers, mosquitoes, bed bugs, thrips, transient rat or bird mites, and mange mites, among others (Fellner & Majeed, 2009; Hinkle, 2011).
Case Examples from Washington State
Case 1
A man complained insects were damaging his cistern, eating the toilet, causing cracks in ceramic, and eating his heroin.
Case 2
An older woman complained that invisible insects were eating the finish off the paint along the cupboards and doorways and eating the paint from her china.
Case 3
A couple made repeated visits to a county Extension office to discuss the insects in their skin. Both were nervous and agitated and had other physical manifestations of methamphetamine use. This couple said they could see the insects streaming out through the enamel of their stove. On one visit, they brought in floor sweepings they said contained the pest that was bothering them. Dead earwigs were present in the floor sweepings, but the clients denied those were the culprits and instead pointed to other pests, which were invisible to all those who examined the sample.
Case 4
A middle-aged man brought in several baggies he said contained examples of the insects he found crawling in his skin. No living organisms could be detected in these samples. He also brought in used bath water for examination and pointed to examples of the bugs in the water, but they could not be seen by others.
Case 5
A health department entomologist had a recurring DI client. Out of frustration on the last call, the entomologist almost decided to not talk to the man, but relented and spent some time with the client again. Several weeks later, the entomologist received a thank you note from the client saying he had intended to kill himself that night, but he finally “heard” what the entomologist was saying and decided against suicide. These cases sometimes can have dire consequences if desperate clients are not heard with compassion and reason.
Discussion
Extension professionals and/or volunteers may encounter individuals potentially afflicted with Delusional Infestation at plant clinics, in office settings, at demonstration gardens, and other work-related settings. The nature of this condition and the behavior of those suffering from it are outside the realm of most Extension-related training and experience. Extension professionals and volunteers who may encounter such clientele should receive training to help them identify such situations and take appropriate steps to help the person. Ideally, volunteers should refer any potential DI clientele to Extension professionals. If no biting arthropods can be detected, Extension should refer clients to a health professional for a medical work-up, diagnosis, and treatment. It may be necessary to repeat this recommendation to the client over multiple visits.
Extension professionals are in a position to help identify situations where biting arthropods are involved and this should be the first cause to rule out in each case. It is not an Extension professional’s responsibility to diagnose a case of DI, but it is his/her duty to become aware of this condition and educate volunteers about it. Extension professionals and volunteers need to be familiar with the signs of DI and have a referral plan for suspected cases.
Another poorly-understood skin condition is called Morgellons (a.k.a. “fiber disease”), which may or may not be a new syndrome or just a variation of DI (Freudenmann & Lepping, 2009). Unfortunately, inaccurate information about DI and Morgellons abounds on the Internet. There are web sites where sufferers share their case histories, theories, and remedies; deride the medical community for its inability to diagnose and treat the problem (Freudenmann & Lepping, 2009); and validate their belief they are afflicted with a legitimate medical condition. When educating the public how to judge the validity of information, stress the importance of critically examining the information’s author, source, date, purpose, supporting links, intended audience, domain name, and references.
Recommendations
When dealing with clients possibly afflicted with DI, Extension personnel should rely on facts and science:
• Put submitted samples under a microscope and look for insects. Let complainants see this effort and let them look for themselves.
• Do not open any container submitted by a potential DI sufferer without first determining what may be in the container. Some may submit blood, scabs, skin scrapings, bodily fluids, and stool samples, which should be handled by trained medical personal.
• Show images of known biting insects for comparison. Explain that insects and other arthropods have characteristic body parts that include segments, head, wings, and legs. Develop a specimen library from past submissions to help clients recognize known biting insects. However, do not be surprised if clients persist in their belief that “bugs” are to blame, regardless of any evidence or explanations presented (Fellner & Majeed, 2009)—this is the very nature of their delusion.
• Provide clients with fact sheets on life cycles of known biting arthropods.
• Explain that some pests (e.g. mites) are microscopic, but not invisible (Figure 3).
• Inquire about pets in the home and pest problems such as nesting animals. Ask questions to help rule out actual biting arthropods.
• Recommend helpful and doable tactics to trap suspected biting arthropods such as setting out water pan traps or glue traps and using clear tape to catch the perpetrators of bites in progress.
• Never agree with clients about their claims, but do not disagree either (Koblenzer, 2010; Lee, 2008; Mehmood & Khasawneh, 2014). Some sufferers will become very agitated and unpredictable when their beliefs are challenged (Freudenmann & Lepping, 2009).
• Never use the word “bites” when talking about the complainant’s skin lesions. One entomologist uses this statement in her reports to presumed DI sufferers: “For issues related to human health (the red welts on your skin), we recommend that you continue to work closely with your doctor to try to determine the cause of the problem. We are not medically trained to do so” (Sharon Collman, personal communication, August 21, 2014). Another says “We are only trained in arthropod identification and cannot diagnose skin lesions” (David Pehling, personal communication, August 21, 2014).
• It is inappropriate and futile for clients to show their “bites” to Extension personnel and volunteers; this should be firmly discouraged. Diagnosis based simply on physical appearance is not possible even by medical professionals. Additional tests must be performed and/or the causal agent isolated before a diagnosis can be made; this is beyond the purview of Extension work.
• After ruling out an actual insect cause, insist the client consult a health care professional qualified to make a diagnosis. An entomologist or trained volunteer can make a statement such as "No arthropods or pests were observed in your samples. Multiple factors can be associated with your discomfort. Although it is best to consider each factor including pests, seek assistance from your primary physician to ease the sensation itself” (Michael Bush, personal communication, August 23, 2014).
• Extension professionals and volunteers should never diagnose clients as delusional or in need of psychological help. Let a properly trained medical specialist do this. Many DI sufferers eventually consult physicians and/or dermatologists, but few follow through with a recommendation to seek psychiatric care (Koblenzer, 2010; Wykoff, 1987; Trabert, 1995; Boggild et al., 2010).
• Create a standard short and direct response letter that includes the non-finding of an arthropod cause. Do not include criticism of their belief or treatment recommendations. Do recommend they consult a physician (Freudenmann & Lepping, 2009).
• Avoid being alone with complainants when possible. Additional witnesses may help prevent confrontations and provide moral support for clients. One Extension entomologist has established this policy: “In our office, I have trained the receptionists to recognize symptoms of someone who potentially suffers from DI. In these cases, they call me or the Master Gardener volunteer to the reception area rather than escort a client back to an office” (Michael Bush, personal communication, September 3, 2014).
• Extension personnel at all county offices and clinics should learn to recognize potential DI cases and have a plan to seek help if a customer becomes assaultive or violent.
• Keep in mind that DI is a human health issue and is outside the scope of most Extension work. An inability to change the client’s convictions or have them accept science-based facts is not a failure on the part of Extension personnel or volunteers. Avoid the tendency to feel frustrated, depressed, or discouraged by the lack of positive outcomes when working with clientele afflicted by DI. Conducting a thorough investigation into the bona fide involvement of biting arthropods and, absent positive findings, suggesting an examination by a medical professional is the best Extension personnel can do in their service capacity.
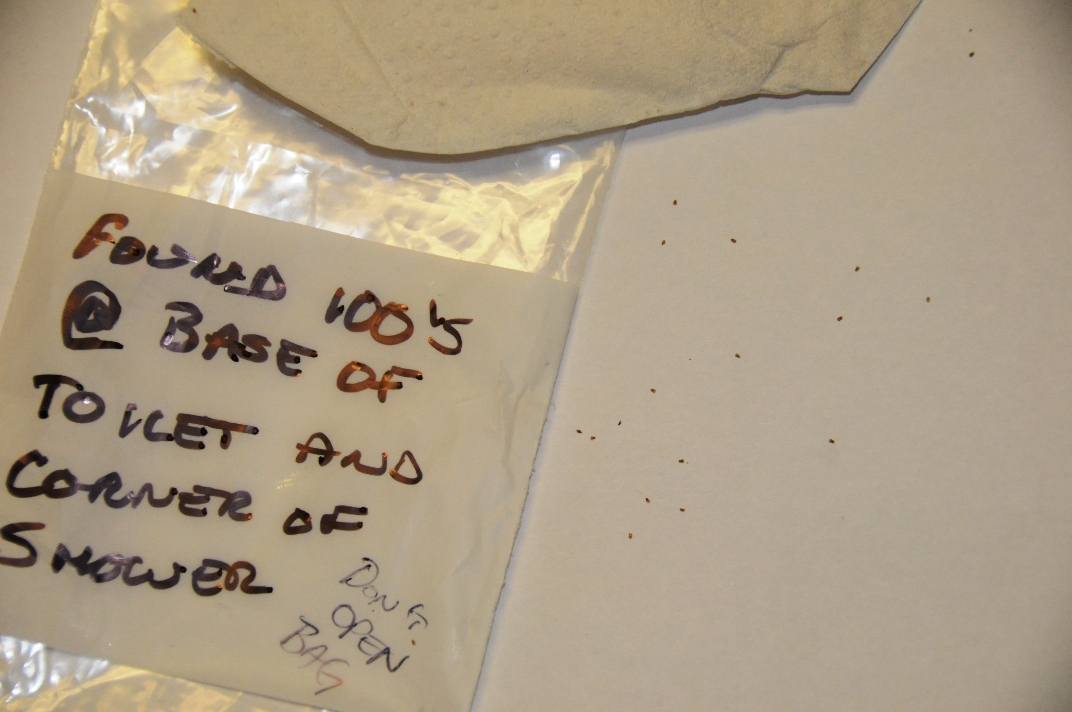
Figure 3. Make a good faith effort to look for biting arthropods. Like these actively-moving bird mites found infesting a client’s bathroom, some biting pests may be microscopic, but not invisible. Photo courtesy of Mike Bush.
Conclusions
Delusional Infestation is a rare condition, but one that Extension personnel may see manifested in clientele multiple times during the course of their Extension career. This condition is disturbing and frustrating for all involved because it is a problem rarely cured without specific psychoactive medication or treatment of the primary cause. When dealing with suspected cases, be prepared to spend considerable time with the client. Extension personnel should remain sympathetic and patient with DI sufferers because these delusions cause great anguish, frustration, fear, and pain in clients. Many sufferers have been struggling with the condition for years and may be on the verge of losing hope. Awareness, advanced training, and protocols to deal with DI cases will help Extension professionals and volunteers prepare for these unusual and potentially-upsetting situations. Extension personnel need to take precautions to keep themselves safe yet do what is best for their clientele.
Helpful Resources Related to This Topic
Diagnosing Mysterious “Bug Bites”
http://citybugs.tamu.edu/factsheets/biting-stinging/others/ent-3006-2
Invisible Itches: Insect and Non-Insect Causes
http://www2.ca.uky.edu/agc/pubs/ent/ent58/ent58.pdf
Delusory Parasitosis: What's Attacking Me?
www.ipm.ucdavis.edu/PMG/PESTNOTES/pn7443.html
Human Skin Parasites & Delusional Parasitosis
http://delusion.ucdavis.edu
Delusions of Parasitosis
http://emedicine.medscape.com/article/1121818-overview
Skin Problems & Treatments Health Center: Morgellens
www.webmd.com/skin-problems-and-treatments/morgellons-disease-what-is-it
Clinical, Epidemiologic, Histopathology and Molecular Features of an Unexplained Dermopathy
www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0029908
Criteria for Evaluating the Accuracy/Validity of a Website
http://usa-document.com/lb/Evaluating%20Websites.pdf
Tropical Rat and Northern Fowl Mites Fact Sheet
www.cdph.ca.gov/HealthInfo/discond/Documents/MitesFactSheet2010.pdf
Literature Cited
Boggild, A. K., Nicks, B. A., Yen, L., Van Voorhis, W., McMullen, R., Buckner, F. S., & Liles, W. C. (2010). Delusional parasitosis: six-year experience with 23 consecutive cases at an academic medical center. International Journal of Infectious Diseases, 14(4), e317–e321. http://dx.doi.org/10.1016/j.ijid.2009.05.018
Fellner, M. J., & Majeed, M. H. (2009). Tales of bugs, delusions of parasitosis, and what to do. Clinics in Dermatology, 27(1), 135–138. http://dx.doi.org/10.1016/j.clindermatol.2008.05.007
Freudenmann, R. W., & Lepping, P. (2009). Delusional Infestation. Clinical Microbiology Reviews, 22(4), 690-732. http://dx.doi.org/10.1128/CMR.00018-09
Frieden, J. (2006). Skin Manifestations May Signal Crystal Meth Use. Family Practice News, 36, 47.
Hinkle, N. C. (2000). Delusory Parasitosis. American Entomologist, 46(1), 17-25.
Hinkle, N. C. (2010). Ekbom Syndrome: The Challenge of "Invisible Bug" Infestations. The Annual Review of Entomology, 55, 77-94. http://dx.doi.org/10.1146/annurev.ento.54.110807.090514
Hinkle, N. C. (2011). Ekbom Syndrome: A Delusional Condition of “Bugs in the Skin.” Current Psychiatry Reports, 13(3), 178–186. http://dx.doi.org/10.1007/s11920-011-0188-0
Koblenzer, C. S. (2010). The Current Management of Delusional Parasitosis and Dermatitis Artefacta. Skin Therapy Letter, 15(9), 1-3. Retrieved from www.skintherapyletter.skin.ca.
Lee, C. S. (2008). Delusions of parasitosis. Dermatologic Therapy, 21, 2–7. http://dx.doi.org/10.1111/j.1529-8019.2008.00163.x
Lyell, A. (1983). Delusions of parasitosis. British Journal of Dermatology, 108(4), 485-499.
http://dx.doi.org/10.1111/j.1365-2133.1983.tb04604.x
Mehmood, M., & Khasawneh, F. A. (2014). Specimen sign. BMJ Case Reports. http://dx.doi.org/10.1136/bcr-2013-202850
Munro, A. (1988). Monosymptomatic Hypochondriacal Psychosis. British Journal of Psychiatry, 153(suppl. 2), 37-40.
Trabert, W. (1995). 100 Years of Delusional Parasitosis. Meta-Analysis of 1,223 Case Reports. Psychopathology, 28(5), 238-246. http://dx.doi.org/10.1159/000284934
Wykoff, R. F. (1987). Delusions of parasitosis: a review. Reviews of Infectious Diseases, 9(3), 433–437.
http://dx.doi.org/10.1093/clinids/9.3.433
Yeh, T., Lin, Y., Chen, L., Chiang, C., Mao, W., Chang, H., Kao, Y., & Tzeng, N. (2104). Aripiprazole treatment in a case of amphetamine-induced delusional infestation. Australian and New Zealand Journal of Psychiatry, 48(7), 681-682. http://dx.doi.org/10.1177/0004867414525849